It’s a sunny spring morning in Adelaide. Joanne Dart is enjoying a coffee in SAHMRI’s stunning atrium with fellow employee, Prof David Yeung; the man she credits for saving her life, and the reason she came to work at the institute in accounting.
“I applied because I love SAHMRI, I love what they do for the community, and I knew David’s connection. I’ve been here for two years now and it’s meant a lot to me,” Jo said.
“I often think about the research that’s kept me alive and is helping so many other people. Without it and without David, I certainly wouldn’t be here.”
The conversation between Jo and David is care-free and comfortable – a far cry from when the two first met 14 years ago.
“The first time I met David, I was still in shock from the news a day earlier that I had leukaemia,” Jo said.
David was her treating physician, and also a postdoctoral researcher specialising in blood cancer.
Jo was 44, working and living happily and healthily in Whyalla, married to Don with two children when she was diagnosed.
“I’d been to my GP for a routine blood test and the results sat there for weeks before anyone looked at them, because my doctor went away on holiday,” Jo said.
“I thought I was perfectly fine, until someone from the Royal Adelaide Hospital called me out of the blue three weeks later and told me I needed to go straight to hospital.”
“It changed my life instantly that phone call.”
Working in a clinical role at the RAH and as a researcher at SAHMRI gives David a dual lens through which to focus on improving treatment efficacy while reducing side effects for patients living with various forms of leukaemia. David, like fellow SAHMRI clinical researchers, including Prof Tim Hughes, A/Prof Dan Thomas, A/Prof Peter Psaltis and Dr Devendra Hiwase to name a few, is delivering world-class health care now, while simultaneously seeking breakthroughs to improve disease prevention, diagnosis and treatment in the future.
“Being a clinician and a researcher, I’m able to see first-hand how the progression of cancer research directly translates to improving patients’ lives, and my research is simultaneously informed by understanding what’s needed in the clinic,” David said.
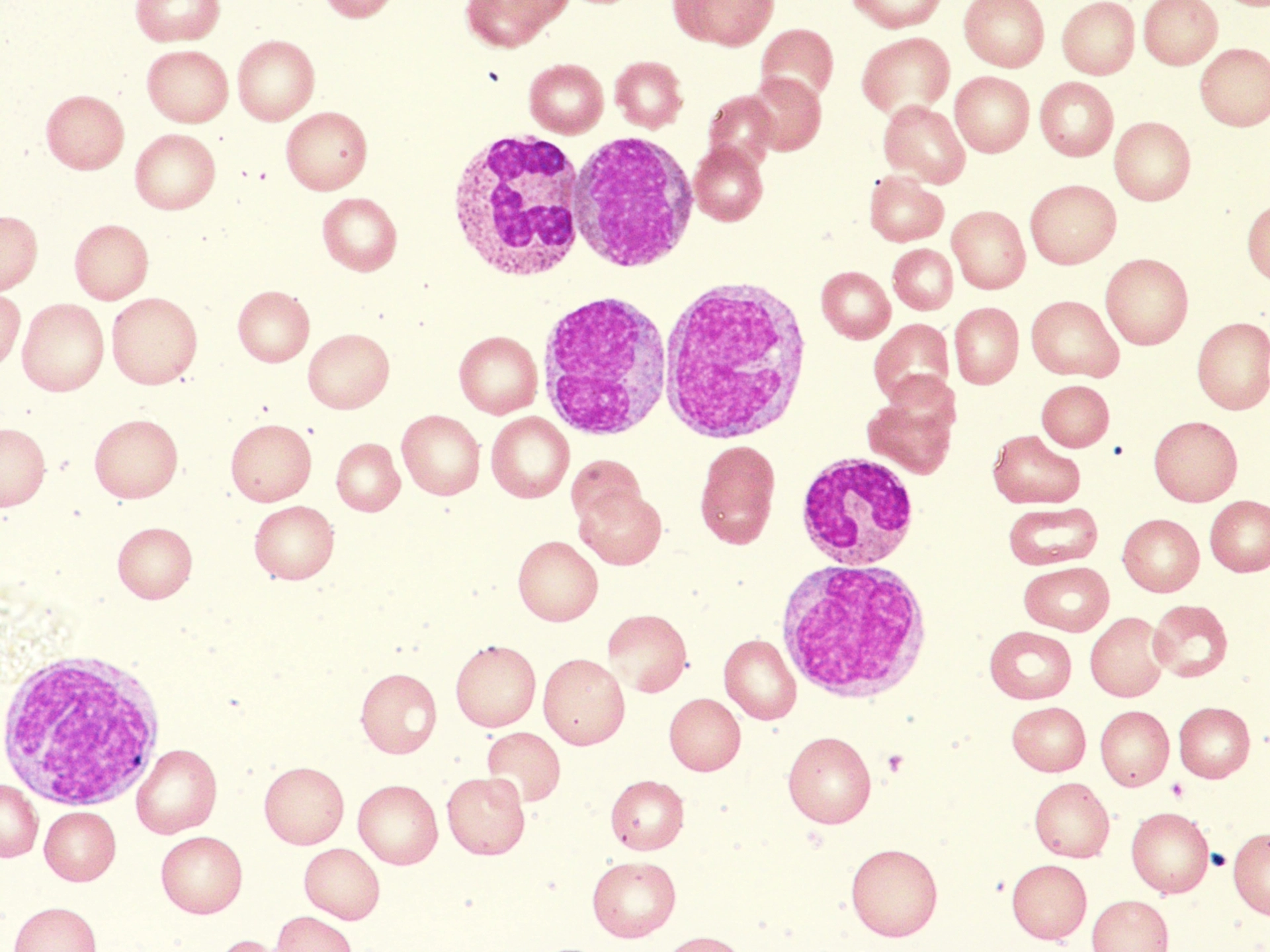
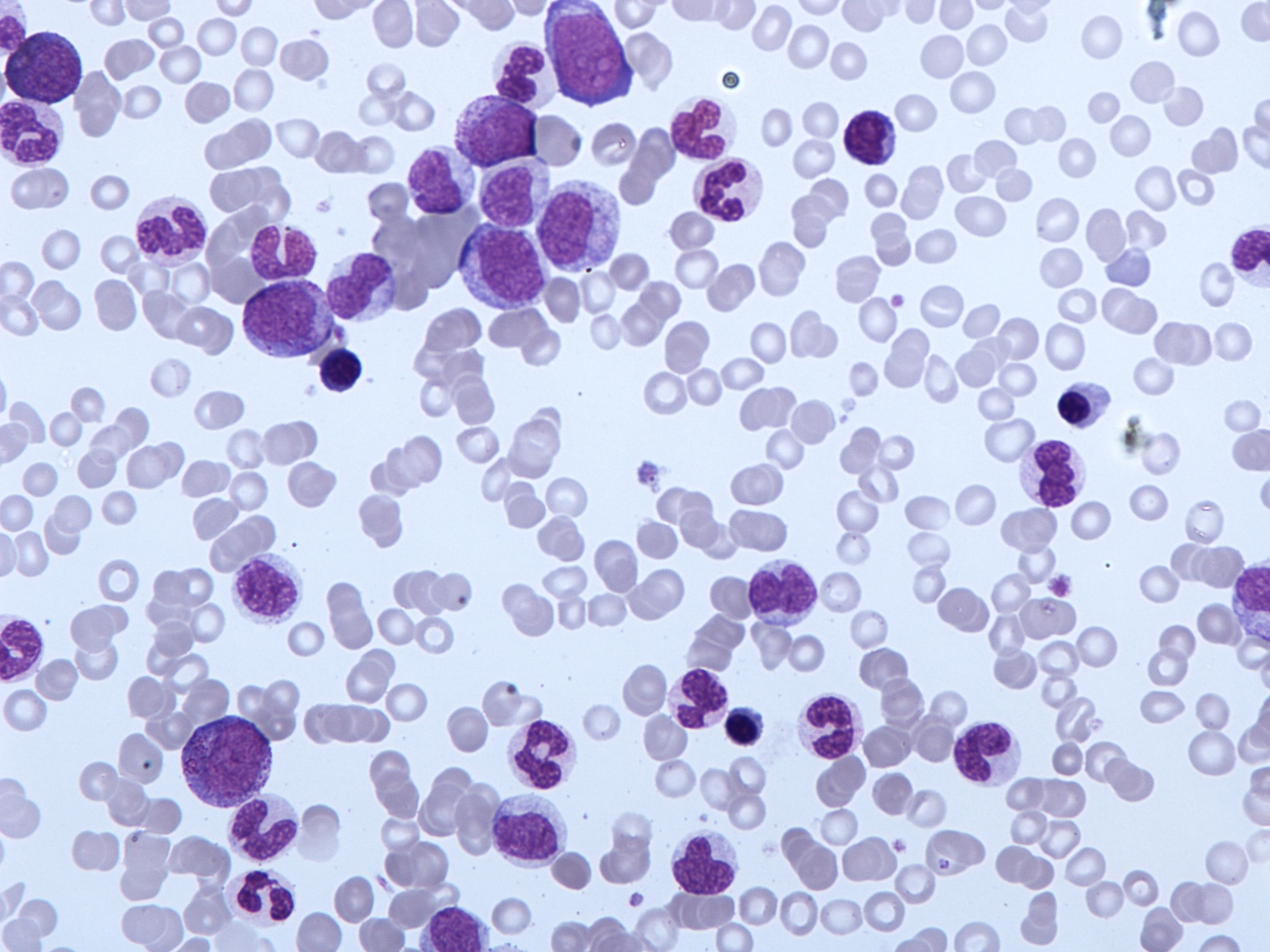
Jo was one of David’s first patients, and both recall their first meeting, when the confronting details of Jo’s diagnosis were laid out. She had acute myeloid leukaemia (AML), a rare and aggressive cancer with the lowest survival rate of all leukaemias.

“I remember meeting Jo and talking about her home, her career and her family. Things that are important to her, and things that she would have to leave behind at the time to concentrate on her battle with cancer,” David said.
“One of the biggest challenges when we meet patients is to get all of the information across in a way they can understand. There’s so much to take on board and it can be very overwhelming.”
Jo recalls trying to process the haze of information.
“I remember David trying his best to explain to me what it was, but I couldn’t take it in,” Jo said.
“I said to him, ‘you can fix this right?’, and he just looked at me and said he’d do his best. That’s when I thought ‘well maybe it can’t be fixed’.”
In 2010, AML research had already made significant strides, to the point where there were treatment options, but the impact of multiple rounds of chemotherapy was in some ways more punishing that the disease itself.
“It was horrendous. I really struggled with the side effects and how many tests there were,” Jo said.
“One moment life’s all on track and you’re happy, the next you're stuck in a hospital room for months on end, not knowing if you’ll ever make it home.”
In the past decade and a half, various new research discoveries have been made to improve patient care. For some forms of leukaemia, targeted treatments sometimes as convenient as taking a tablet are now available as an alternative to chemotherapy.
“Some cancers can be treated with targeted drugs either by themselves, or paired with chemotherapy to make treatment less toxic, so patients don’t have to endure as many side effects,” David said.
“For other types of leukaemia, the mainstay of treatment is still combination chemotherapy, but by and large, the conversations we have with families now are more optimistic and hopeful.”
In the midst of her cancer battle, Jo suffered a secondary infection in her leg muscles. It was brought on by her body’s severely lowered immunity and compounded by an allergic reaction to an antibiotic. The combined effect landed her in the ICU and nearly proved fatal.
“I was scared. There were moments when I was really sick where I thought that might be it,” Jo said.
“It’s a whole different world you have to give yourself over to and the trust factor is huge, I trusted David 100 percent. We had a connection right from the start. He was honest, open and friendly and despite everything, we laughed.”
Under David’s guidance, Jo made an astounding recovery, returning to Whyalla and slowly put the pieces of her life back together.
“David told me he really wanted to give me one more round of chemo just to be sure; that’s when I zipped up my bag and said, ‘thanks but no thanks, I’ll take my chances’,” Jo said.
“On reflection I should’ve taken more time to process everything that happened, but I was in such a rush to get back to normal. And I did get back normal. How lucky am I?!”
Jo’s been in treatment free remission ever since, but still sees David for check-ups every year.
“He’s still my go-to to this day. If I ever have anything serious done medically, I won’t agree to it unless they call David first,” Jo said.
David values his personal relationship with Jo but humbly deflects credit for her recovery.
“It’s the whole team,” David said.
“Our multidisciplinary approach across research and clinical care really is one of the hallmarks of SAHMRI and what makes it such an essential part of our healthcare ecosystem.
“If leukaemia research continues on this trajectory, we’ll be able to offer people longer life and better quality of life during treatment and in post cancer care.
“I think we’ll progress to the point we don’t need to do stem cell transplants to keep patients in remission anymore.”
Despite the growing capacity to treat blood cancer more effectively and save lives, the incidence of new cases continues to rapidly increase, rising by just under 50% in the past decade.
The latest statistics from the Leukaemia Foundation show around 135,000 people are living with blood cancer or a blood disorder in Australia today, with that number expected to double again by 2035, making the research effort more important than ever.