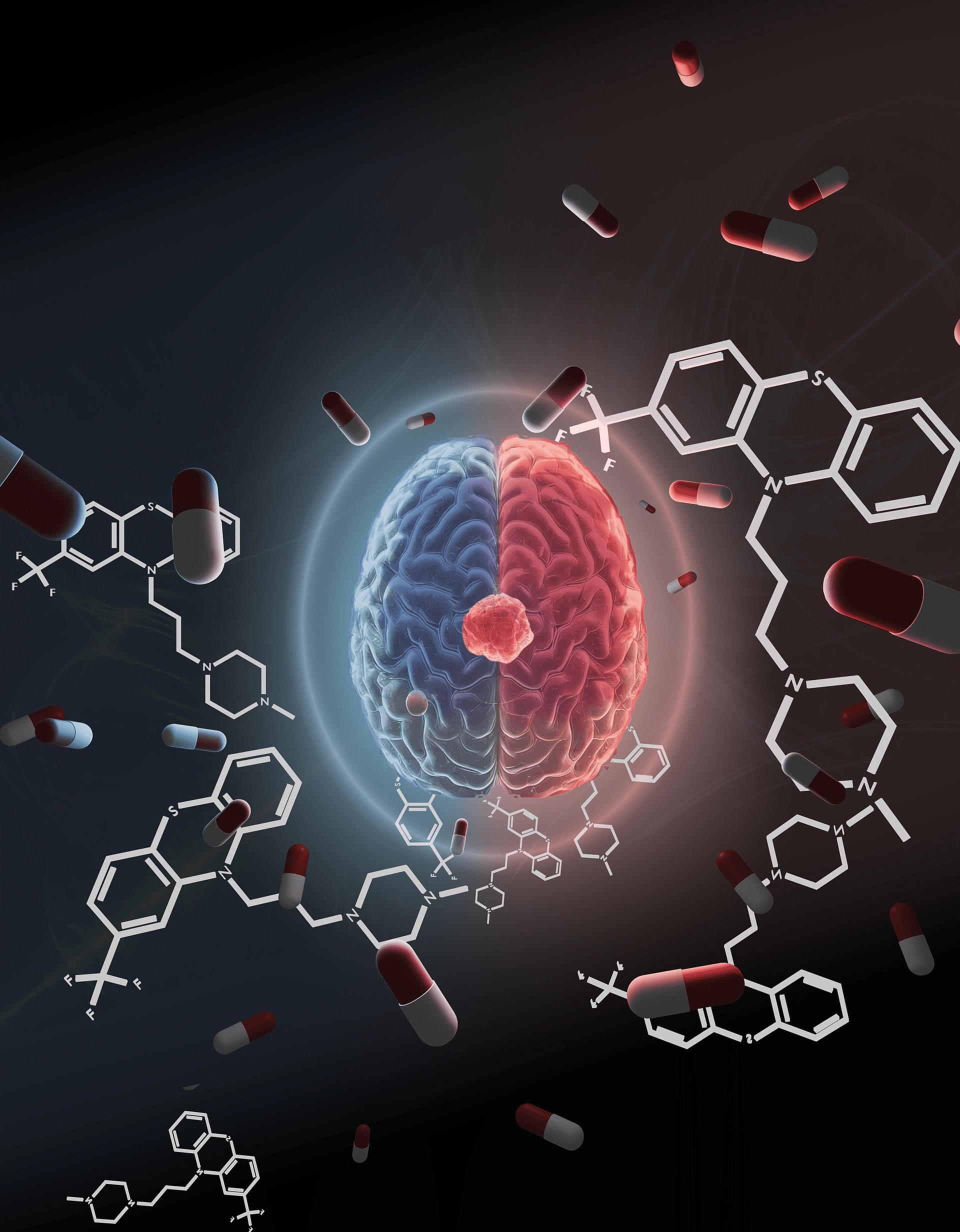
New research from SAHMRI and Flinders University has shed light on how decades-old antipsychotic drug, trifluoperazine (TFP), works against glioblastoma (GBM), the most aggressive form of brain cancer.
Previous studies from Professor Cedric Bardy’s Laboratory for Human Neurophysiology and Genetics at SAHMRI, have shown TFP can kill GBM cells effectively.
Now the group’s latest review, published in Trends in Pharmacological Sciences, has uncovered the reason why the drug is such an effective tool in helping to combat GBM treatment resistance.
Lead author, Dr Inushi De Silva, says the findings provide critical insight into how the underlying mechanisms of TFP could be used to improve current GBM therapies.
“GBM cells have dopamine receptors, and TFP targets these receptors, disrupting pathways that allow the tumour to adapt and grow,” Dr De Silva said.
“The drug also affects a transcription factor called NUPR1, which is linked to treatment resistance in GBM and other cancers like pancreatic cancer. By targeting this pathway, TFP may help make existing treatments, such as temozolomide, more effective.”
While TFP has been FDA-approved since the 1950s as an antipsychotic, its potential as a cancer treatment remains largely unexplored. A small clinical trial in the 1990s investigated its effects on GBM but was limited by poor study design.
Dr De Silva hopes the new findings will provide the foundation for further clinical trials.
“GBM is difficult to treat because the tumour cells can shift between different states to evade therapy,” she said.
“Most treatments target a single pathway, but GBM finds a way around it. TFP is different because it acts on multiple mechanisms at once, which could make it harder for the cancer to escape.”
With more research, scientists hope TFP could be repurposed to complement existing therapies and improve outcomes for GBM patients.
“This study reinforces the drug’s potential and gives us a clearer picture of how it works. The next step is securing funding for clinical trials to explore its role in treatment,” Dr De Silva said.
Professor Bardy says current standard treatments for glioblastoma are simply not good enough on their own, with median survival stagnating around 15 months.
“New adjunct therapies preventing cancer cells from evading chemotherapy and radiotherapy are urgently needed. Trifluoperazine might be able to help with that,” Prof Bardy said.
“A key benefit of this being an old drug given to people with anxiety, is that its side effects are predictable. If future clinical trials prove its efficacy in brain cancer patients, this could transform glioblastoma treatment very rapidly.”