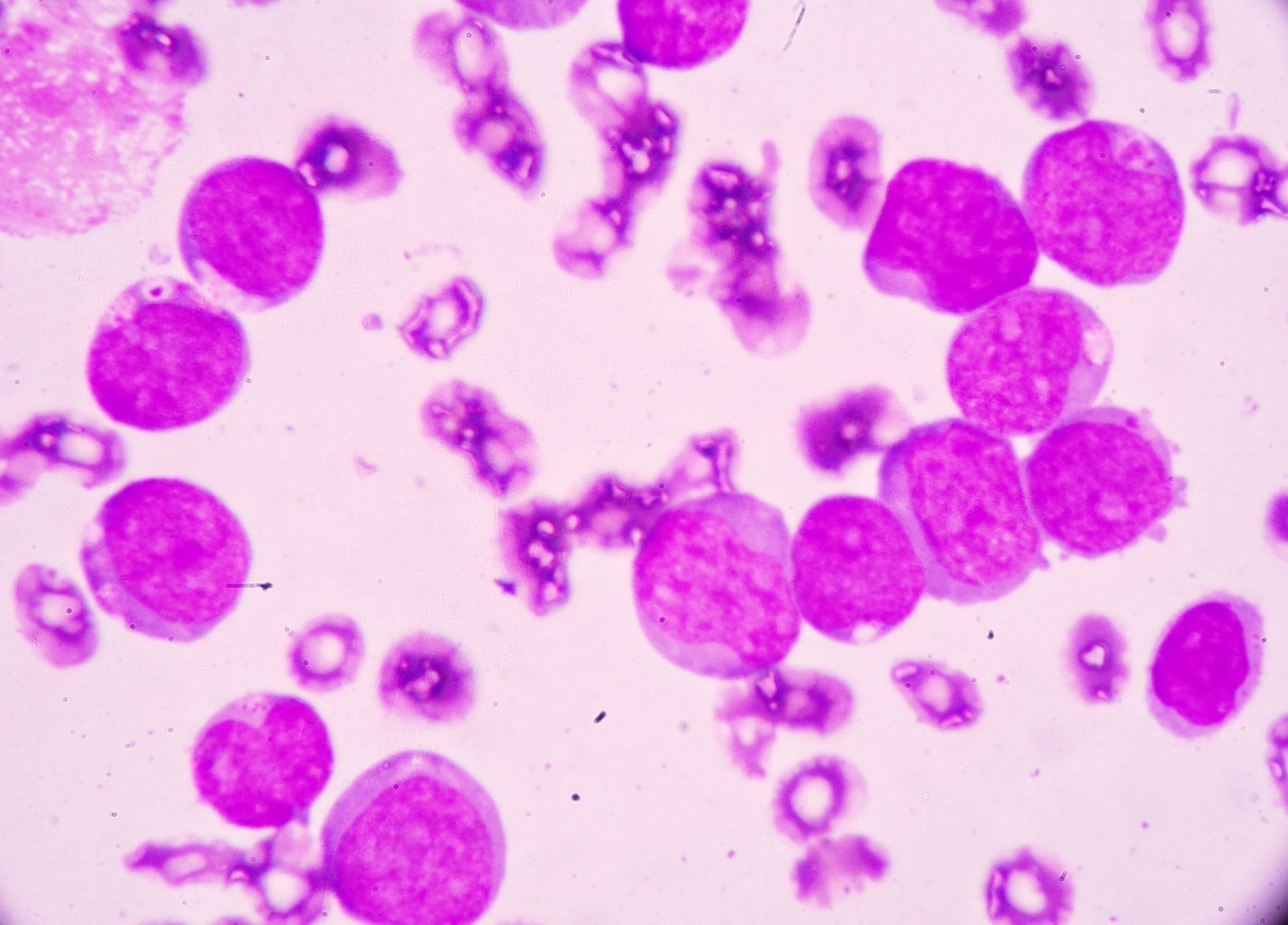
A revolutionary medication to treat chronic myeloid leukaemia (CML) could become the new frontline therapy for people newly diagnosed with the once-fatal blood cancer.
Asciminib (known by the brand name Scemblix) was developed by Swiss multinational pharmaceutical corporation, Novartis, and validated by international clinical trials led by SAHMRI's Professor Tim Hughes.
The drug works by blocking the action of an abnormal protein that signals cancer cells to multiply and was designed to be both highly potent and specific, minimising side effects and toxicity.
Following the 2021 success of the world-first clinical trial based in Australia, the drug has just been put to the test in a phase III global randomised control study.
The study involved 405 men and women with a median age of 52, who’d been recently diagnosed with CML. They were treated with either asciminib or an older tyrosine kinase inhibitor (TKI) therapy, to compare treatment efficacy and safety.
Presenting the findings at the American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago, Prof Hughes says the latest trial results showed asciminib is an overall superior option for people with new cases of CML compared to current standard treatments.
“We’re excited, because this trial demonstrates that asciminib achieves statistically superior efficacy and importantly, safety and tolerability was also excellent,” he said.
“Asciminib could soon become the treatment of choice for many newly diagnosed CML patients. That’ll mean people can stay at work, they can stay productive, and we’ll see significantly more achieving treatment free remission.”
Treatment of chronic phase CML requires the long-term use of TKIs to prevent the disease from progressing to a more aggressive phase. However, around half of all patients will need to switch TKIs if the CML stops responding to treatment or if the treatment cannot be tolerated due to side effects.
Between 10% and 20% of patients have significant intolerance to TKI therapy, which may not improve after switching to a different medication.
To measure how well treatment worked, researchers assessed individual’s major molecular response (MMR). Patients who have an MMR are more likely to have CML that is well controlled and reaching MMR early is also a predictor of better long-term outcomes.
“After 48 weeks, 68% of participants on asciminib had achieved an MMR compared to 49% on other TKIs,” Prof Hughes said.
“A deep molecular response was also observed in 39% of those taking asciminib in comparison to 21% in the control group. People who have a deep molecular response may eventually be considered in remission and could stop treatment.”
“Additionally, asciminib has shown lower rates of discontinuation, dose adjustment and treatment interruptions, indicating better tolerance. It also all but eliminated the threat of blood clots, a severe side effect of TKIs, present in only 1% of participants who took asciminib.”
Researchers will continue to follow the participants to understand the long-term safety of asciminib and determine if reaching an earlier MMR continues to be a way to predict better outcomes for patients.
Future studies will measure overall survival, progression-free survival, and whether treatment-free remission is reached.